What are bedsores?
Bedsores – otherwise known as pressure ulcers – are caused when a part of the body is continually compressed so that blood flow is restricted due to remaining in the same position for a long time. The skin becomes reddish and sore and can lead to the onset of bacterial infections and serious infection or even death. Most common among the bedridden, bedsores occur when a patient is unable to turn over by themselves due to dementia or paralysis.
Severity of pressure ulcers
| Stage Ⅰ | Redness and intradermal bleeding that does not disappear even when pressure is applied to the skin. |
| Stage Ⅱ | Friction causes the skin from Stage 1 so that it peels off, exposing the dermis layer and forming blisters. |
| Stage Ⅲ | Tissue defects extend to the subcutaneous tissue. |
| Stage Ⅳ | Tissue defects extend beyond the fascia to muscles, bones and tendons and are susceptible to infection. |
Stage classification advocated by NPUAP (American Pressure Ulcer Questionnaire)
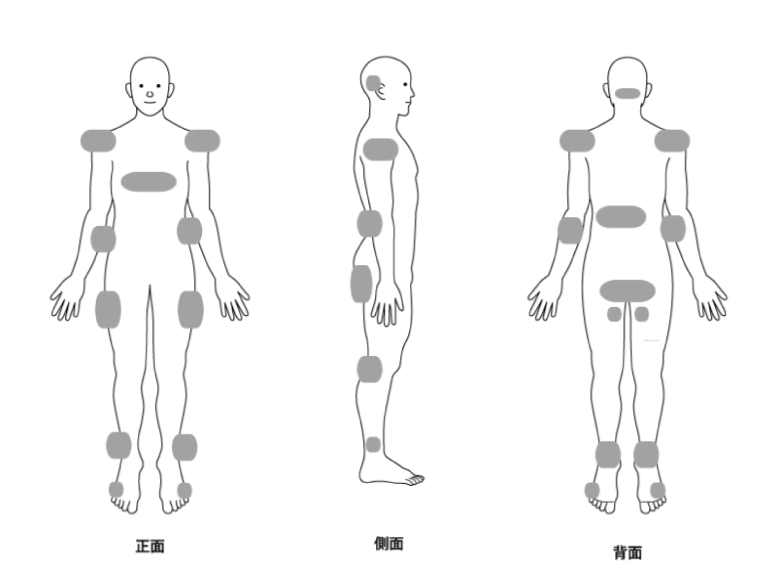
Location of bedsores
Bedsores form easily on protruding parts of the bone where pressure is applied continuously, most commonly on the central bone of the sacral buttocks when a patient is sleeping on their back. When sleeping sideways, bedsores are more likely to occur on the outside of the base of the thigh of the greater trochanter.
Four major causes of bedsores
- Pressure
Those who cannot turn over on their own, who have contractures or paralysis in their joints, or who are thin, are more likely to have more pressure on certain areas and are more likely to develop bedsores.
- Friction
Friction is another cause of bedsores. If there are wrinkles in the sheets or clothes and the patient does not move, there is likely to be a restriction of blood flow that can also lead to a build-up of pressure in certain points of the body. Friction can also occur when the patient is moved from a bed to a wheelchair. This too can weaken the skin and lead to bedsores.
- Sanitation
Sanitation is another root cause of bedsores. Patients who use diapers or who have trouble controlling their body temperature may become sweaty or unsanitary, and this can also lead to an environment conducive to the formation of bedsores.
- Undernourishment
Undernourishment reduces resistance and healing power, leading to deterioration of a patient’s general condition. This weakens the immune system and makes it easier for pressure ulcers to develop.
Preventing bedsores
Once bedsores occur they can be difficult to heal, which is why a preventative approach is most often adopted. It’s important to check the patient’s skin regularly to ensure there are no obvious pressure points that could form into problem areas.
- Posture change
While paying attention to the parts that are likely to be prone to bedsores, change the direction and posture of the body regularly so that the same part of the body is not pressed in the same position for a long time. If you see redness on your skin, try to change your position.
- Use bedsore prevention equipment
Air mattresses and pressure distribution tools are available to alleviate the formation of bedsores.
- Prevent skin friction and slippage
Choose clothing that is soft to the touch and has good breathability, and when moving your body, be careful not to drag it to prevent friction on your skin. Also, prevent wrinkles and seams such as sheets and sleeping clothes from directly hitting the skin.
- Keep your body clean
Bathing is great for improving blood circulation and is also effective for prevention of bedsores. If it is difficult to take a bath, take a partial bath.
- Maintain good nutrition
Keep in mind a well-balanced diet and proper hydration can help with your body’s ability to fight infection. If your diet is small, make sure you eat nutritious foods.
About the treatment of bedsores
The most important treatment is to clean and treat the wound site with an appropriate ointment. However, it is even more critical to properly identity the cause of bedsores in order to prevent recurrence.